This post was written based on an appearance by Dr. Matthew Bartock, hematology and oncology, Parkview Packnett Family Cancer Institute, on the show PBS HealthLine.
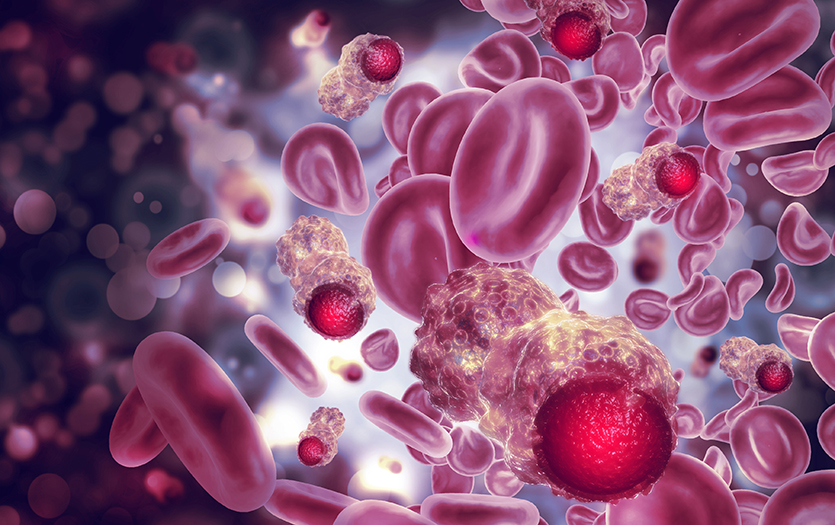
Blood cancer affects millions of people each year, yet it remains misunderstood by many. In this post, we demystify this complex group of diseases and answer questions about diagnosis, treatment and daily life with blood cancer.
What Is blood cancer?
Blood cancer isn’t just one disease, but a broad category that includes several types of cancers affecting blood cells, bone marrow or the lymphatic system. These include:
· Leukemias – cancers of the blood and bone marrow
· Lymphomas – cancers that usually begin in immune system cells
· Myeloma – a cancer of plasma cells
· Pre-leukemic disorders – conditions that may lead to leukemia in some cases
Each type behaves differently and may require a different treatment approach.
How common is blood cancer?
About 1.2 million people are affected by blood cancers each year in the United States, and because diagnostic tools are improving, more cases are being found at earlier stages. Blood cancers can occur at any age, from childhood leukemias to myeloma in older adults.
Causes and risk factors
While some risk factors are known, such as exposure to certain chemicals (like benzene, herbicides and agent orange), radiation or prior chemotherapy, often there is no identifiable cause for why someone develops blood cancer. Genetic mutations that arise randomly during cell division are a frequent culprit. Smoking and obesity may elevate risk, but many patients with blood cancer don’t fit any obvious risk profile.
Signs and symptoms to watch for
Not every patient experiences noticeable symptoms early on. In some cases, blood cancers are detected during routine blood work before symptoms appear. But some people do present with what are called “B symptoms,” which are:
- Fevers
- Night sweats
- Unintentional weight loss
How blood cancers are diagnosed
Diagnosis typically begins with blood tests, which may show abnormal cell counts or shapes. From there, doctors may perform imaging studies or a bone-marrow biopsy, where a tiny sample of marrow is taken for detailed analysis, to determine the type and extent of disease.
Treatment options and advances
Treatment depends on the specific disease and its severity. The main approaches include:
· Chemotherapy – Traditional chemotherapy targets rapidly dividing cells, including cancerous ones, but can also affect healthy cells.
- Targeted therapy – Certain blood cancers have specific genetic markers, and newer medications can target those mutations directly, often with better results and fewer side effects.
- Immunotherapy – This strategy boosts the immune system’s ability to recognize and kill cancer cells.
- Stem cell transplants – For diseases like leukemia and myeloma, bone-marrow or stem-cell transplants may be used to replace diseased bone marrow with healthy cells after intensive treatment.
- CAR-T therapy – A breakthrough cancer treatment that reprograms a patient’s own immune cells to recognize and attack blood cancers like leukemia, myeloma and lymphoma. By engineering these T cells in a lab and infusing them back into the body, doctors can unleash a highly targeted immune response that has led to remarkable remissions in some patients who had run out of other options.
Living with and beyond blood cancer
Many blood cancers are now treatable, and in some cases curable, especially when diagnosed early or when effective targeted therapies are available. Other types may become chronic conditions that patients live with for years thanks to ongoing medical advances. Before these medical advances, patients with some of these conditions were exposed to harsher, more toxic therapies and prognosis was considered to be grim.
It’s important to build a strong care team and listen closely to your body. You also need support from family and friends, whether they’re driving to appointments, helping with chores or simply offering a listening ear, it makes a meaningful difference.
Final thoughts
Understanding the basics — from risk factors and symptoms to diagnosis and treatment — empowers patients and caregivers to navigate the journey ahead with more confidence. With continuous research and evolving therapies, there is growing hope for improved outcomes and a higher quality of life for those living with blood cancer.
If you're experiencing the symptoms detailed above, reach out to your primary care provider to have a discussion about your health.
Don't have a primary care provider? Call (877) PPG-TODAY to get connected with one.



