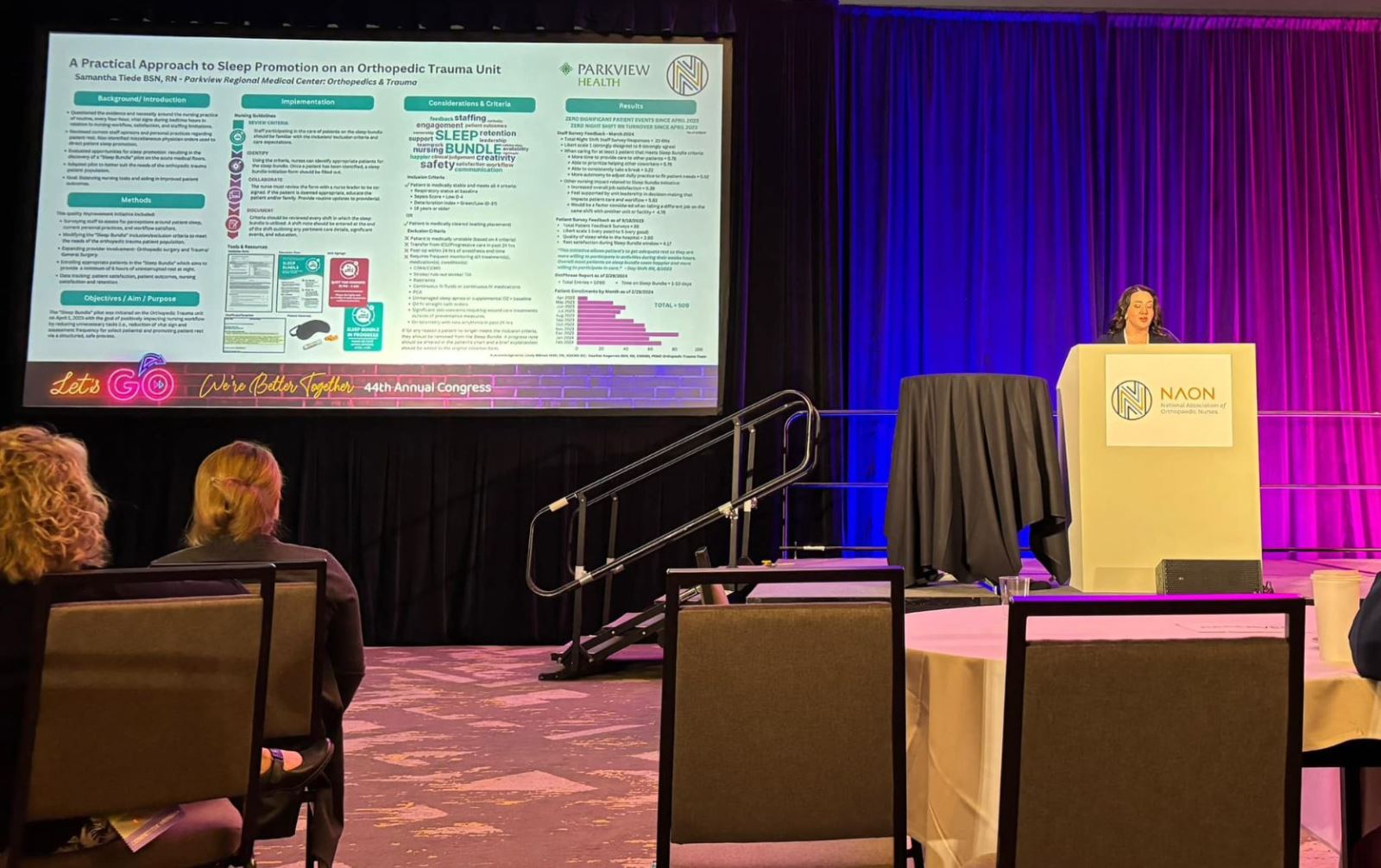
In 2023, Samantha Tiede, BSN, RN, assistant nurse manager, Parkview Health, led the Sleep Bundle quality improvement project in Parkview's Orthopedic Trauma unit to reduce unnecessary overnight vital sign checks. In this post, she shares how those measures ensure patients get more restful sleep and support night shift nurses during times of limited staffing.
Night shift challenges
When we started this initiative, it was also important to me that we focus on the impact current care expectations had on our night shift nurses. Night shift can sometimes be harder to staff, and team members are managing high workloads with fewer hands.
I knew I couldn't magically create more co-workers overnight, but I believed there had to be creative, meaningful ways to ease the load while still prioritizing patient care. That mindset led me to partner with Jan Powers, Director of Nursing Research, and Lindy Bilimek, Clinical Nurse Specialist, as well as my direct leadership team, to explore current practices. After extensive consideration, we homed in on one routine that didn't sit right with the team, which was waking stable patients every four hours for vital signs.
Concept development
The idea stemmed from a simple but essential question: "Are we waking patients more than we need to?"
In most acute care settings at Parkview, it's common practice to check vital signs every four hours, day or night. While routine monitoring helps catch early signs of deterioration, it often means waking patients at night, interrupting their much-needed rest. We recognized that these frequent checks, especially for clinically stable patients, were disrupting sleep without always adding value.
From there, we adapted a Sleep Bundle framework to fit our unique patient population. I led the unit's efforts to implement it, from designing the process and tools to educating co-workers and tracking our outcomes.
Benefits for patients and caregivers
We found that reducing non-essential interruptions not only helps patients get more rest but also improves their sleep quality. This, in turn, leads to faster recovery and lowers the risk of complications, such as delirium, especially in older adults. Fewer disruptions also contribute to a more positive overall hospital experience.
Moreover, adopting this model also gives nurses more time to focus on patients with complex care needs, improves workflow, and reduces unnecessary strain.
Addressing potential risks
It's worth noting that there's no substantial evidence to support every 4-hour vital signs as the gold standard for all patients. What really makes the difference is thoughtful, individualized nursing assessment and critical thinking. By shifting the focus from routine to intentional, we're prioritizing both safety and rest.
That said, not all patients are suitable candidates for the Sleep Bundle. We start by identifying patients who are clinically stable and meet clear inclusion criteria:
-
Respiratory status at baseline
-
Sepsis Score = Low 0-4
-
Deterioration Index = Green/Low 0-37)
-
18 years or older
If, for any reason, a patient no longer meets the inclusion criteria, they are removed from the Sleep Bundle. Nurses are also encouraged to use their clinical judgment and can always opt out of reduced checks if there's any concern.
Outcomes and feedback
Feedback from both patients and co-workers was overwhelmingly positive. During the early stages of the project, we conducted surveys with both groups. Patients reported better sleep, and nurses appreciated the ability to individualize care using their clinical judgment.
Furthermore, several day shift nurses even noted that patients who were on the Sleep Bundle during the night seemed more energized and engaged in daytime care activities, such as physical therapy.
Closing reflections
What began as a response to staffing challenges has grown into a practice that not only promotes patient rest but also contributes to better nurse satisfaction and workflow balance.
Personally, the project reminded me that sustainable change doesn't always require sweeping reforms; sometimes it starts with small, thoughtful adjustments that make daily work more manageable and patient care more compassionate.
Professionally, this experience strengthened my leadership skills in a way that felt deeply connected to bedside nursing. It allowed me to uplift the voice of clinical nurses and translate their feedback into action. In fact, we went nearly a year without a single night shift nurse leaving the team after the project began. While improving workflow likely played a role, it also highlights something even more powerful. When nurses are trusted to make informed decisions for their patients, outcomes tend to speak for themselves.
It reinforced my belief that when nurses are empowered to question and innovate, the benefits ripple outward for patients, staff and the overall culture of the unit. I'm proud of what we've accomplished and grateful for the opportunity to continue growing these efforts.




